Scoliosis
What is scoliosis?
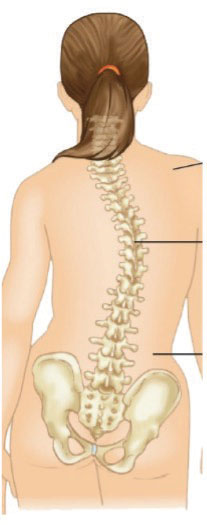
Scoliosis is a common condition that affects many children and adolescents. Simply put, it is a curvature of the spine. When viewed from the front, a spine usually looks like the letter “I”. A spine with scoliosis curves to the right or the left, looking more like the letter “C” or “S”. Scoliosis often develops during puberty when kids are growing very quickly. Small curves occur in boys and girls equally, however, girls are more likely to go on to develop larger curves that need to be treated.
Often times, a curve will initially get discovered at a school screening or a regular check-up with the pediatrician. It is rarely associated with pain, and kids with scoliosis are still able to do all the activities and sports that kids without scoliosis can do.
What does scoliosis look like?
- Uneven shoulders
- Curved back
- Uneven waist
- Appearing to lean to one side
- A bump on the back appears when leaning forward
Why does scoliosis happen?
Scoliosis can occur for several reasons. The most common types are:
- Congenital: If there is an issue with the development of the bones of the spine before a baby is born, this can cause a curve in the spine.
- Neuromuscular: Certain medical conditions such as cerebral palsy or muscular dystrophy can lead to muscle imbalances. These imbalances can lead to the development of curves in the spine.
- Idiopathic: This is the most common type of scoliosis. “Idiopathic” means unknown, though now we know it is mostly based on genetics. These curves tend to develop during adolescence but can also occur in toddlers and younger children too.
How is scoliosis treated?
If there is a concern for scoliosis, your physician will order x-rays to investigate further. The x-rays will allow your doctor to measure any curves in the spine, as well as see how much bone growth is still possible. As scoliosis tends to be a condition of growth, this is important to consider!
Depending on the degree of the curve and growth remaining for the child, the doctor will determine the best treatment options.
| Maturity/Severity |
Mild
(10-25 degrees) |
Moderate
(25-45 degrees) |
Progressive
(>45 degrees) |
| Significant growth potential |
Observation |
Bracing |
Surgery |
| Little growth potential |
Observation |
Observation |
Surgery |
Scoliosis curves fall into 4 categories:
- Spinal Asymmetry (less than 10 degrees): About 10 percent of the population has a very small curve, less than 10 degrees, which is called spinal asymmetry. This does not require any treatment at all.
- Mild curves (10 to 25 degrees): In most cases of scoliosis, the curves are mild. Regardless of how much growth is left, the only treatment needed is observation. Your doctor will monitor the curve on a regular basis with x-rays, usually every 6-12 months.
- Moderate curves (25 to 45 degrees): If the curve falls into the moderate category and your child is almost done growing, the treatment is still observation. Since there is not much growing left, it is unlikely that it will get worse, and your doctor will monitor the curve with x-rays on a regular basis.
- If there is still a significant amount of growth left, your doctor may recommend bracing. The brace is called a TLSO, and it is specially made to fit your child. Periodically your doctor will take x-rays and check how the brace is fitting. Bracing will not straighten out the curve but has been found to help prevent a moderate curve from becoming progressive if it is worn as directed. Once there is little growth potential left, bracing is usually discontinued.
- Progressive curves (greater than 45 degrees): Large curves, also called progressive curves, typically require a surgery called “posterior spinal fusion”. This is because without stabilization the curve can continue to worsen, leading to less space in the chest and breathing problems too.
- Surgery will help to restore a more normal posture and prevent worsening of the curve. If your child needs an operation the doctor and his team will go over all the particulars and be there with you every step of the way.
Reviewed by: Stephen G George, MD
This page was last updated on: March 14, 2024 04:14 PM